What is - Axial Spondyloarthritis (Ankylosing Spondylitis)

Spondyloarthritis (SpA) is an arthritic condition that affects the joints of the spine, causing inflammation, severe pain and stiffness in the back. SpA can also affect the joints, digits and tendons in the upper and lower limbs as well, and may occasionally cause inflammation of the eye (uveitis), skin (psoriasis) and intestines (eg. Crohn’s disease, ulcerative colitis).
Axial spondyloarthritis concentrates on the axial skeleton - chest, spine, and pelvis. Some of the conditions included under SpA are ankylosing spondylitis (AS), psoriatic arthritis (PsA), anterior uveitis and inflammatory bowel disease. AS is the prototype for SpA with mainly spinal involvement, thus the following information shall focus on purely on AS.
The spine and its vertebrae are divided into three main segments: the cervical (neck), thoracic (chest), and lumbar (back). AS often affects the sacroiliac joints and lumbar segments first although the neck and thoracic segments can also be affected. As the condition progresses, the inflammation may cause fusion of the spine and in some cases
the entire spine may become fused resulting in complete rigidity of the spine, a condition known as “bamboo spine”. When this occurs, the patient may experience difficulties in turning his head or bending forward to put on his shoes.
Generally, ankylosing spondylitis affects 1 per 500-1000 people, who are mainly in their teens and 20s. It is two to three times more common in males than females. Family members of affected people are at higher risk, depending partly on whether they inherited the HLA-B27 gene.
Symptoms of Axial Spondyloarthritis (Ankylosing Spondylitis)
The first signs of AS are pain and stiffness in the lower back. This is especially bad in the morning on getting up. This is quite different from back strain which is better with rest. Occasionally, this may be associated with pain in the hips and knees.
As the condition progresses, the pain and stiffness can affect the entire spine and last the whole day. This causes difficulty in walking, getting out of bed, bending forward and other activities of daily living. Patients with active AS often experience fatigue, poor appetite and weight loss. Occasionally, the eyes can also be affected in AS and the symptoms include redness of the eyes, increased sensitivity to light and blurred vision.
Axial Spondyloarthritis (Ankylosing Spondylitis) - Causes and Risk Factors
Ankylosing spondylitis is hereditary. The major gene that causes this disease is HLA-B27. Almost 90% of people with ankylosing spondylitis are carriers of HLA-B27.
Other risk factors include history of skin psoriasis, uveitis, inflammatory bowel diseases, and reactive arthritis in the patient or his family members. Having the HLA-B27 does not mean that you will develop AS. Only 1-5% of HLA-B27-positive individuals in the general population develop AS.
Diagnosis of Axial Spondyloarthritis (Ankylosing Spondylitis)
Your doctor will review your family medical history and conduct a physical examination especially of your spine and your limbs. If your doctor suspects that you may have this condition, you may be required to perform blood
investigations and X-rays of your spine. X-ray changes of the sacroiliac joints, known as sacroiliitis, is a key sign of spondyloarthritis. If X-rays do not show enough changes, but the symptoms are highly suspicious, your doctor may perform magnetic resonance imaging (MRI) on you, which are able to show these joints better and can pick up early involvement.
Treatment for Axial Spondyloarthritis (Ankylosing Spondylitis)
Specialised and dedicated AS clinics may result in better outcome. Treatment of AS is focused on alleviating symptoms and managing the progression of the condition, to regain and maintain the mobility of the spine and reduce of inflammation in the joints, digits and tendons of the upper and lower limbs.
a. Medication
Although most medications prescribed treat only the symptoms of AS, there is evidence that NSAIDs (non-steroidal anti-inflammatory drugs) may reduce the rate of disease progression in the spine NSAIDs are also important to reduce inflammation, pain and stiffness of the digits, joints and tendons in your upper and lower limbs. Other
pain relieving drugs may also be used.
Depending on the joints involved and the severity of the condition, steroids and DMARDs (disease-modifying
anti-rheumatic drugs) may be prescribed to reduce the inflammation of your joints. In patients who respond poorly to NSAIDs and DMARDs, you may be considered for biologic therapy.
The current approved biologic therapy for AS includes the TNF alpha blockers. They are very effective in treating both the spinal and peripheral joint symptoms of SpA. These drugs are injected subcutaneously (under the skin) or may require infusion in the hospital at regular intervals.
However, anti-TNF treatment is expensive and not without side effects, including an increased risk for serious infections, eg development of active tuberculosis in patients with latent TB.
Your doctor will discuss the cost and weigh the benefits and risks with you when considering treatment with biologic therapies.
b. Exercise
Exercise, including stretching, helps reduce stiffness of the spine and limbs.
Generally, swimming is recommended for all forms of arthritis. Other physical therapies must be recommended and approved by a rheumatologist in consultation with a physiotherapist. In order to be effective, all exercises need to be done regularly and on a long term basis.
Axial Spondyloarthritis (Ankylosing Spondylitis) - Other Information
Ankylosing Spondylitis has a variable course. In some patients the disease is mild and limited to the lower back or spine. In others the whole of the spine can be involved including many of the larger joints like the hips and knees.
In the advanced stage the following complications can develop:
- Destruction of joints in the upper or lower limbs, especially the hip joints
- Heart complications eg. inflammation of the aortic valve of the heart
- Osteoporosis, with increased risk of spinal fracture
SpA is a life-long illness but most people are able to lead normal and productive lives. The most important aspect for the management of this condition is early diagnosis - therefore one must not neglect any backache or back stiffness lasting for more than three months.
If you have SpA, you can help yourself by doing regular exercises like swimming and stretching, adopting a healthy life-style, and most importantly, take your medicine regularly as advised by your doctor. You may want to join a support group with activities such as group physiotherapy/exercises.
The above is also available in Mandarin for further reading:
Contributed by
The information provided is not intended as medical advice. Terms of use. Information provided by SingHealth.
Our Medical Specialists
Get to know our doctors at SingHealth Hospitals in Singapore.
Get to know our doctors at SingHealth Hospitals in Singapore. here.
Our Medical Specialists
1
2
3
4
5
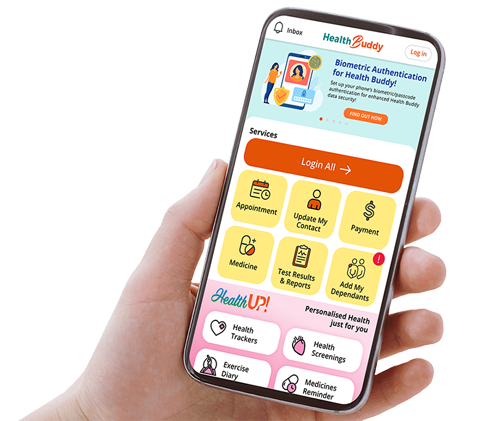
Health Articles