What is - Thalassaemia
What is thalassaemia?
 Haemoglobin is the component in red cells that is responsible for transporting oxygen from the lungs to all parts of the body. Normal haemoglobin comprises two α globin chains and two β globin chains, and each of these protein chains carry an iron-containing haem group which binds to oxygen.
Haemoglobin is the component in red cells that is responsible for transporting oxygen from the lungs to all parts of the body. Normal haemoglobin comprises two α globin chains and two β globin chains, and each of these protein chains carry an iron-containing haem group which binds to oxygen.
Haemoglobinopathies are a group of inheritable conditions which affect the quantity and/or structure of the haemoglobin. The most common haemoglobinopathy in Singapore and Southeast Asia is thalassaemia.
In each individual, there are four α genes (two inherited from each parent) and two β genes (one inherited from each parent). They signal the production of the α globin chains and β globin chains respectively in haemoglobin.
Persons with thalassaemia mutations of the α globin genes (α thalassaemia) have reduced production of α globin chains and those with thalassaemia mutations of the β globin genes (β thalassaemia) have reduced production of β globin chains, resulting in decreased quantities of haemoglobin.
Symptoms of Thalassaemia
What are the symptoms of thalassaemia?
The symptoms and complications of thalassaemia will depend on its severity. This is determined by the number of globin genes involved and the type of thalassaemia mutations.
Persons with thalassaemia trait could have mild anaemia but usually do not have symptoms or complications from thalassaemia. These persons may have only one β globin gene affected by thalassaemia (β thalassaemia trait) or at most two α globin genes affected by thalassaemia (α thalassaemia trait).
Non-transfusion Dependent Thalassaemia
Persons with non-transfusion dependent thalassaemia (NTDT) would usually have moderate anaemia and may experience intermittent symptoms of anaemia such as giddiness or breathlessness as well as intermittent transfusions. They usually experience enlargement of the liver and spleen which may sometimes cause abdominal discomfort. They may also develop other complications related to the thalassaemia, such as high blood pressure in the lungs which can cause breathlessness and decreased effort tolerance. Extra sites for production of haemoglobin outside of the bone marrow such as in the spine can cause back pain, lower limb weakness and numbness. They may also develop ankle/foot ulcers. Persons with NTDT may have both β globin genes mutations, causing only a mild decrease in the production of β globin chains. Hb H disease is when three α globin genes are mutate.
Transfusion Dependent Thalassaemia
Persons with transfusion dependent thalassaemia (TDT) would usually have severe life-threatening anaemia, and require regular blood transfusion for survival from less than 2 years old. Persons with TDT would usually have both β globin genes affected by severe mutations, resulting in absent or negligible β globin chains.
Bart's Hydrops Fetalis
As α globin chains are also needed to produce foetal haemoglobin, foetuses with all four α globin genes affected by thalassaemia mutations would have a very severe form of α thalassaemia, known as Bart's hydrops fetalis. Without intervention, foetuses with Bart's hydrops fetalis usually die during the pregnancy or soon after birth. The mother carrying the foetus with Bart's hydrops fetalis may also experience serious complications.
Thalassaemia - How to prevent
How is thalassaemia prevented?
Thalassemia is a genetic condition and cannot be prevented.
Screening for thalassaemia in couples who are planning to have children or are expecting a child is recommended. If both parents carry the same type of thalassaemia mutations (i.e. both have α thalassaemia or both have β thalassaemia) they are at risk of having children with clinically significant thalassaemia. Antenatal testing of their foetuses for thalassaemia mutations may be carried out by the foetal maternal specialists using specialised procedures.
Thalassaemia - Causes and Risk Factors
What causes thalassaemia?
Thalassemia is a genetic condition and is caused by mutation in the genetic material of cells that make haemoglobin which is involved in the transportation of oxygen. This mutation can be passed from parents to their children.
Diagnosis of Thalassaemia
How is thalassaemia diagnosed?
Initial screening for thalassaemia involves blood tests such as
- Full blood count to look for low haemoglobin level and other abnormal red cell features
- Haemoglobin electrophoresis and HPLC (high performance liquid chromatography) to detect abnormal types of haemoglobin or abnormal proportions
- Genetic testing, especially for confirming α thalassaemia trait.
Treatment for Thalassaemia
How is thalassaemia treated?

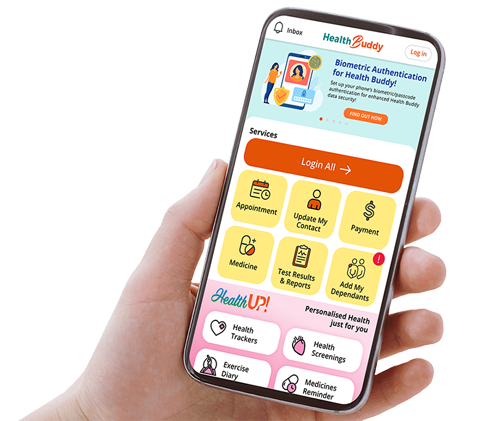
In SGH, we have a specialist Thalassemia Clinic with a dedicated multidisciplinary team consisting of doctors, nurses and social workers.
NTDT patients will need regular monitoring for complications. Some may need intermittent blood transfusion when there are exacerbations of anaemia during pregnancies, infections, or in preparation for surgeries. Some may also need more regular transfusions for specific periods of their lives to prevent or treat complications associated with the thalassaemia such as delayed growth and development. They may develop iron overload from increased gut absorption, and/or transfusions which can affect the heart, liver and endocrine system. Medications are available to chelate iron to prevent the adverse impact on the functions of these organs.
TDT patients need regular blood transfusions every 3- to 5-weekly. They also need regular monitoring for complications from iron loading as a result of the frequent transfusion. Iron chelation therapy is needed to prevent the adverse impact of the iron on the functions of the heart, liver and endocrine system. Haematopoietic stem cell (HSC) transplant is potentially curative and may sometimes be carried out on TDT patients if there is an eligible matched HSC donor (usually a sibling). Such transplants are usually performed during childhood when the transplant outcomes may be better. Gene therapy is another potentially curative treatment that is studied – it currently remains experimental in most parts of the world.
Contributed by
The information provided is not intended as medical advice. Terms of use. Information provided by SingHealth.
Get to know our doctors at SingHealth Hospitals in Singapore.
Get to know our doctors at SingHealth Hospitals in Singapore. here.